The Future of MLTC Quality Reporting
Elevate Your MLTC Program Performance
Hexplora empowers Managed Long-Term Care Plans (MLTC Plans) serving New York Medicaid beneficiaries by seamlessly integrating with the New York State Uniform Assessment System (UAS) to provide invaluable insights. Our analytics solution offers comprehensive visibility into members’ health risks and care costs, enabling proactive interventions and performance improvement. With continuous quality measures monitoring and deep utilization insights, hexplora supports data-driven decision-making, helping MLTC Plans deliver impactful care while meeting financial goals.
Take the next step in data exploration
Key Capabilities
A Comprehensive Analytics
Solution For MLTC Quality Reporting
Automated UAS integration
Effortlessly connect with the New York State Uniform Assessment System, ensuring seamless data access.
STARS & quality measure analytics
Gain valuable insights into STARS program performance and identify areas for quality improvement.
Member risk & cost visibility
Unveil clear data on member health risks and associated costs, enabling proactive care management strategies.
Utilization management tools
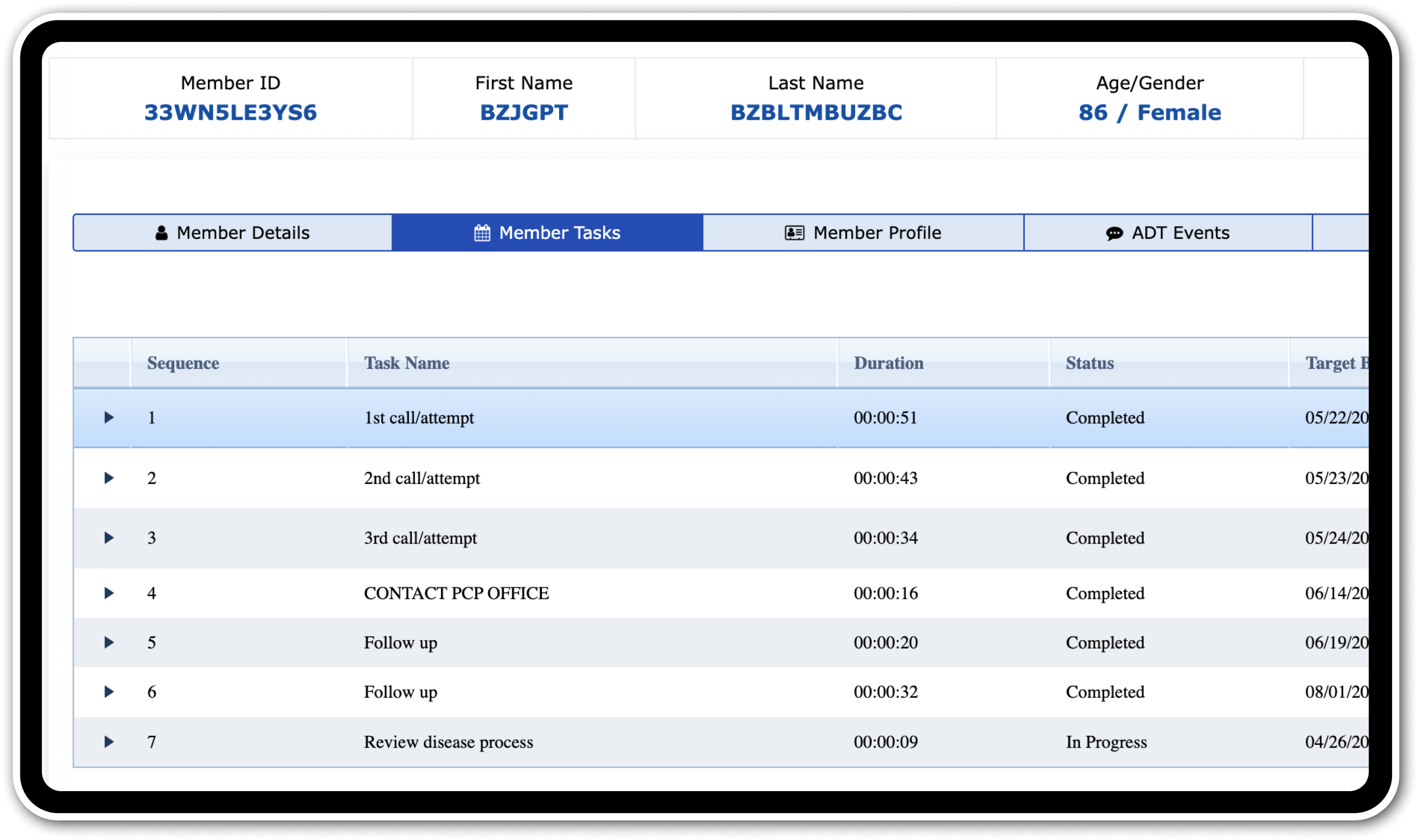
Optimize member utilization through in-depth analytics and informed interventions.
Advanced trend discovery
Uncover hidden trends and potential interventions within complex patient data, empowering proactive care coordination.
Customizable reporting
Generate reports tailored to your specific needs, facilitating clear communication and collaboration across care teams.
