Maximize Medicare Advantage Revenue With Accurate
Risk Adjustment
Your End-to-End Solution For Capturing Full Patient Risk
Medicare risk adjustment plays a crucial role in determining reimbursement for medicare advantage plans. However, accurate coding often takes a backseat to patient care, leading to missed revenue opportunities. Hexplora bridges this gap with a comprehensive solution for managing HCC codes, risk scores, and gaps.
Platform Capabilities
Ensure Optimal Reimbursement & Patient Care
Targeted care programs
Identify and stratify patients for disease-specific interventions.
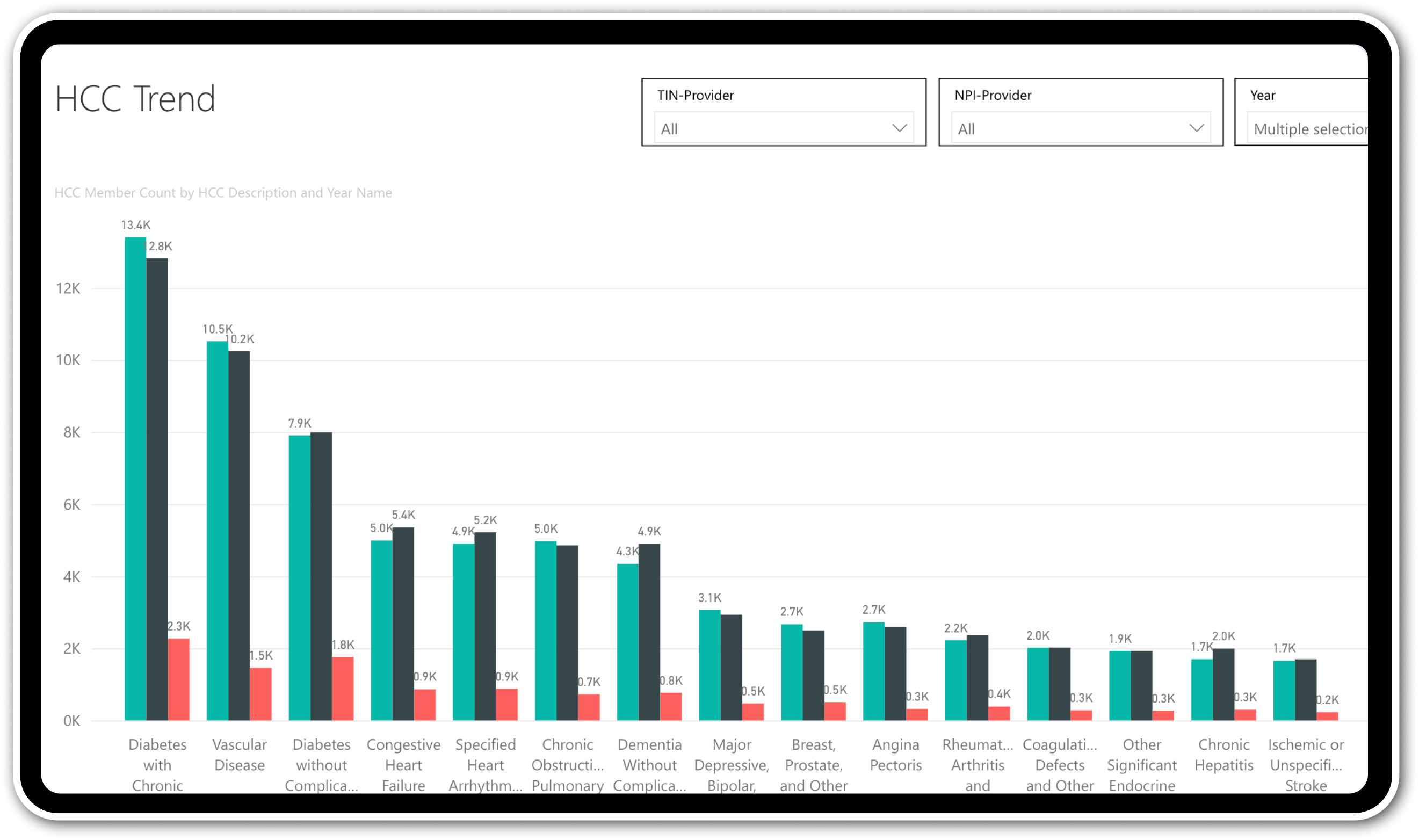
Data-driven insights
Track trends in disease prevalence, comorbidities, and risk scores.
Proactive gap closure
Intelligently identify missing HCC codes for maximized reimbursements.
Financial transparency
Gain insights into risk-adjusted costs and utilization trends.
Accurate forecasting
Forecast and reconcile HCC revenue with confidence.
Seamless compliance
Leverage built-in support for current and past CMS HCC models.
Unlock key insights download datasheets to drive strategic actions
Key Features
Maximize HCC Revenue & Reduce Costs
- Identify and close HCC gaps
- Targeted risk adjustment campaigns
- Collaborative care with providers
- Accurate CMS revenue forecasting
- Our intelligent system finds missed diagnoses in historical data and potential codes based on specialist visits.
- We help you identify chronic and acute conditions, potential comorbidities, and possible HCC conditions linked to quality measures.
- Use this data to target high-risk patients and recapture lost revenue.

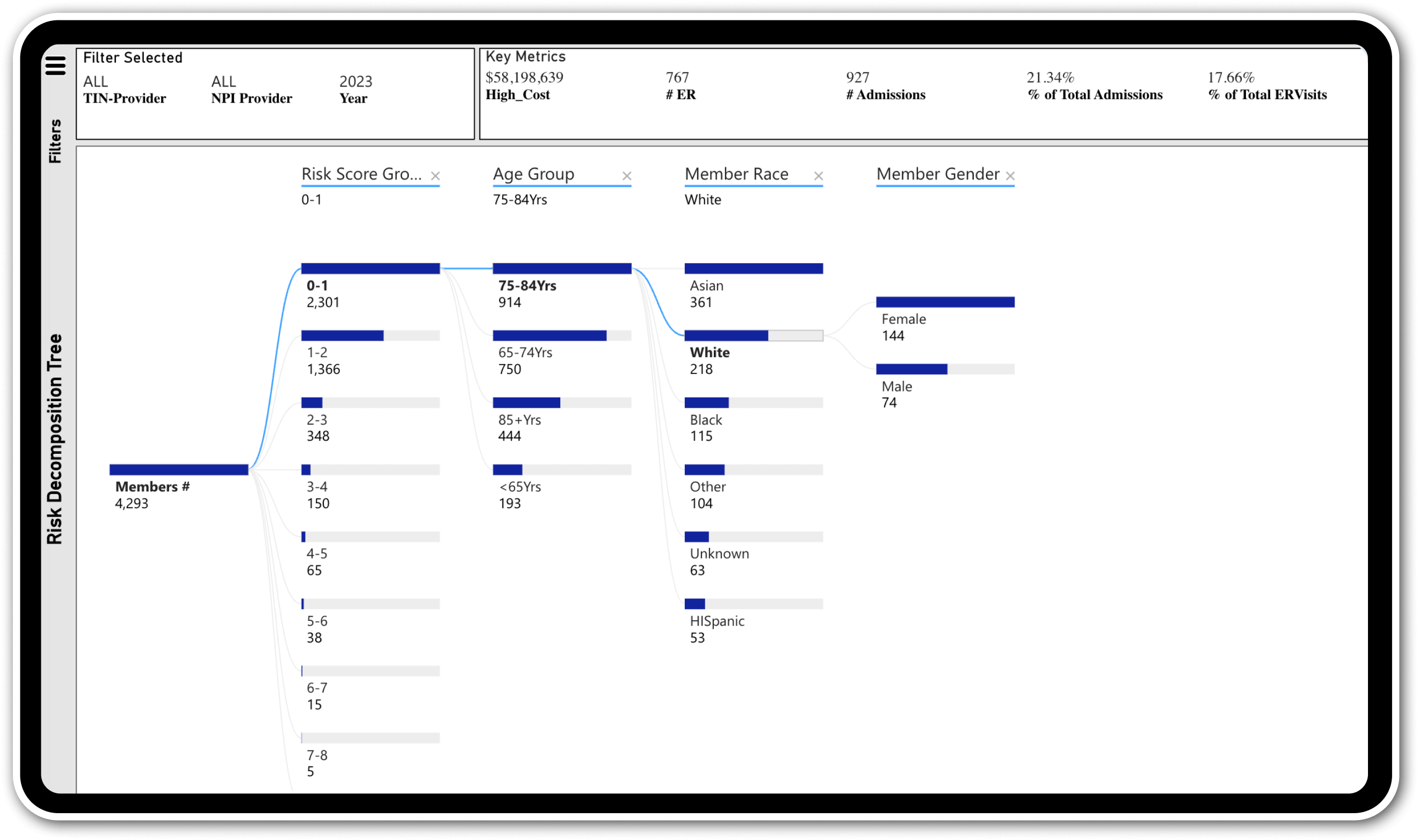
- Create custom member cohorts based on risk scores, diseases, demographics, and costs.
- See the potential impact of interventions on risk scores, recapture rates, and revenue.
- Launch targeted campaigns to optimize risk adjustment efforts.

- Providers can track patient HCC risk scores and identify diagnosis gaps directly in the portal.
- Secure role-based access ensures providers see only assigned patients.
- A guided review process streamlines gap validation for accurate risk capture.

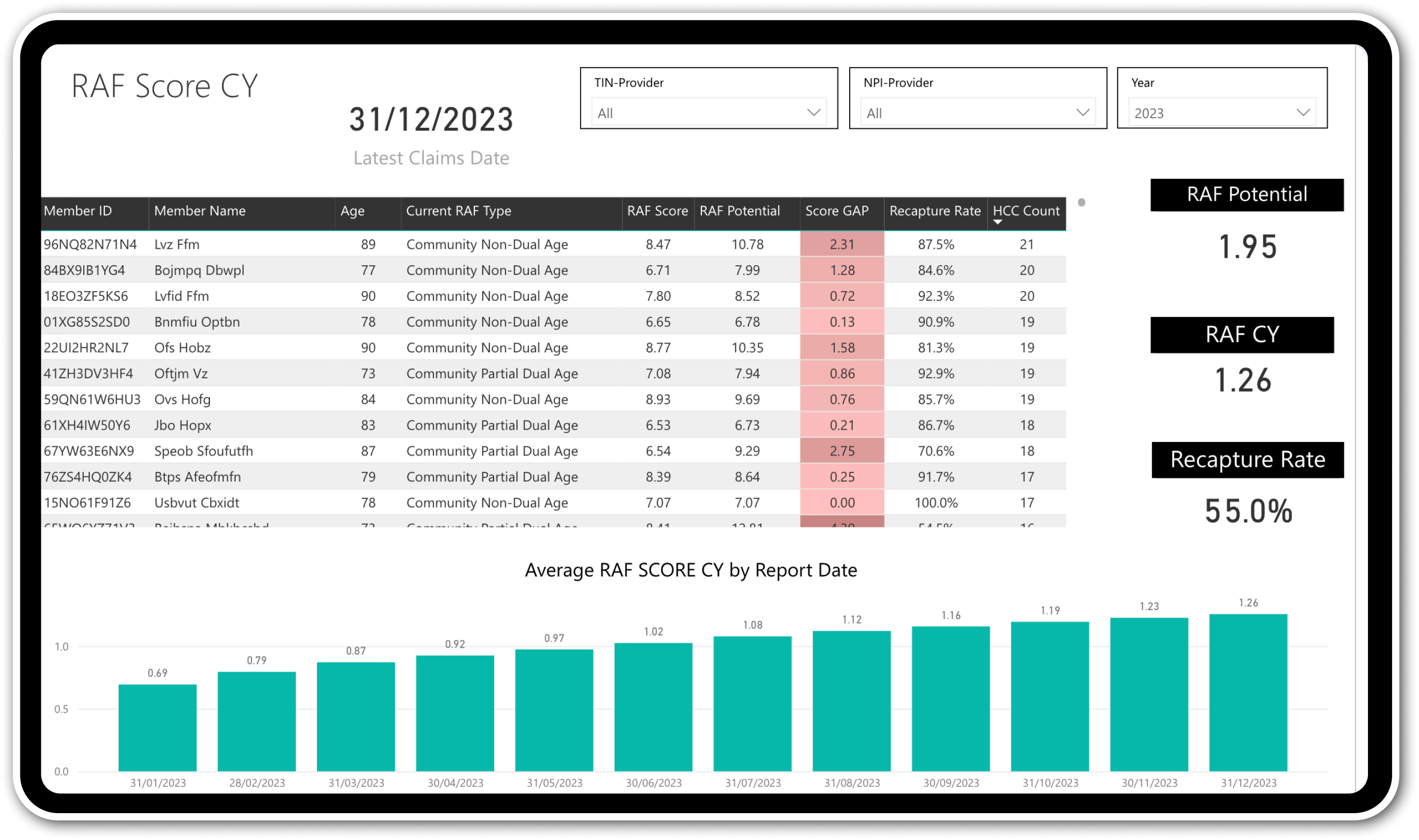
- Get monthly forecasts of CMS reimbursements based on year-to-date diagnoses.
- Reconcile forecasts with actual payments to identify potential adjustments.