Enhancing Healthcare Quality Through Comprehensive
Hedis Reporting Solutions
Demystifying
HEDIS Reporting
Hexplora, a HEDIS-certified vendor, offers a comprehensive quality management solution for health plans to monitor quality measures across all business lines. Our platform supports HEDIS, STARs, and state-specific medicaid measures, aiding in HEDIS reporting challenges with predictive analytics and seamless data integration. With accurate quality measure rates and care gap identification, hexplora promotes collaboration between health plans and providers, leading to meaningful outcomes. Through our portal, providers can effortlessly track and monitor quality measures and care gaps for their patients, improving care delivery.
Take the next step in data exploration
Key Capabilities
Robust Data
Aggregation & Integration
Proactive monitoring & gap identification
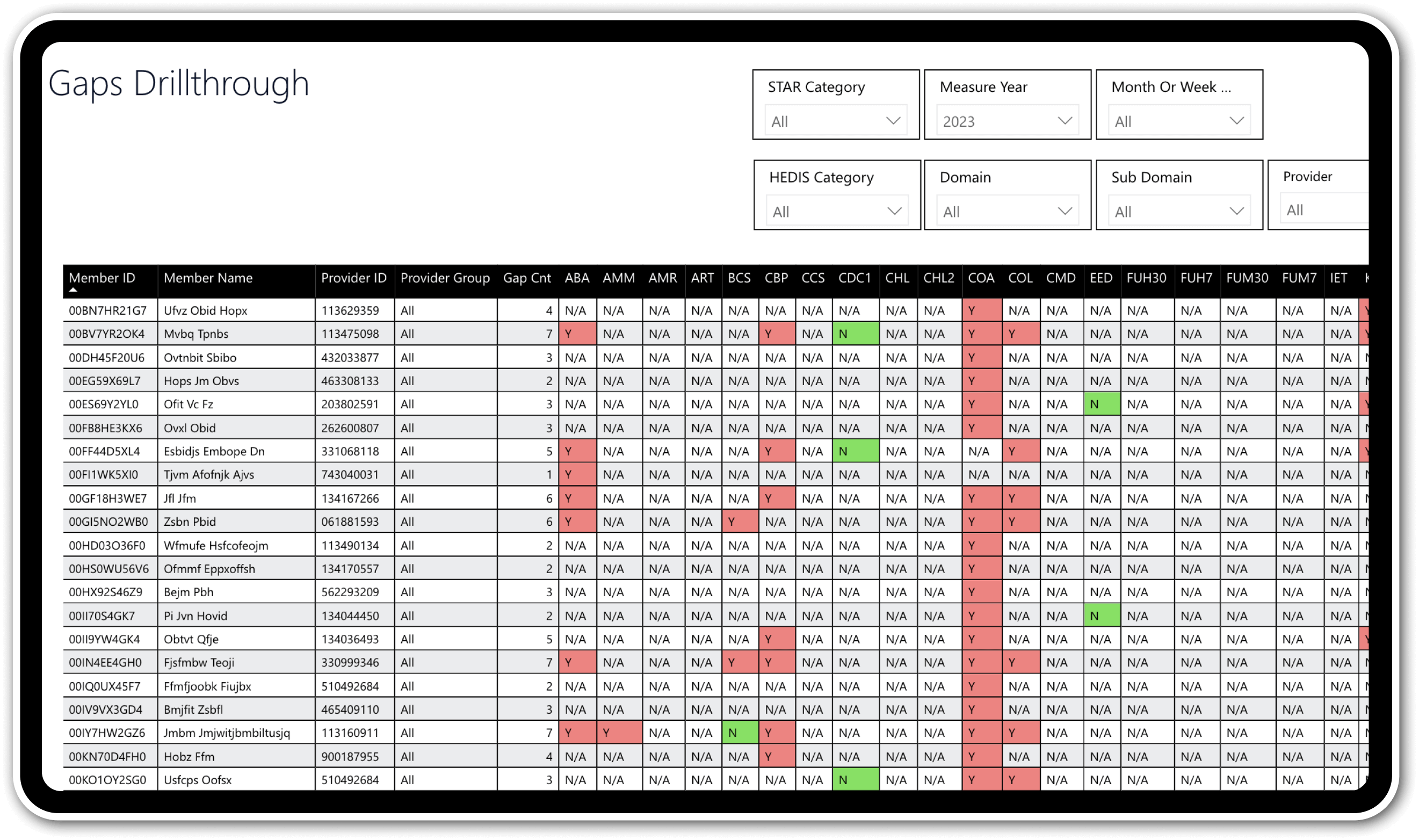
Continuously monitor HEDIS, stars, and other quality measures, proactively identifying and tracking care gaps for timely interventions.
Cost & utilization analytics
Leverage comprehensive analytics to track cost and utilization trends by measure, empowering data-driven decisions to optimize resource allocation.
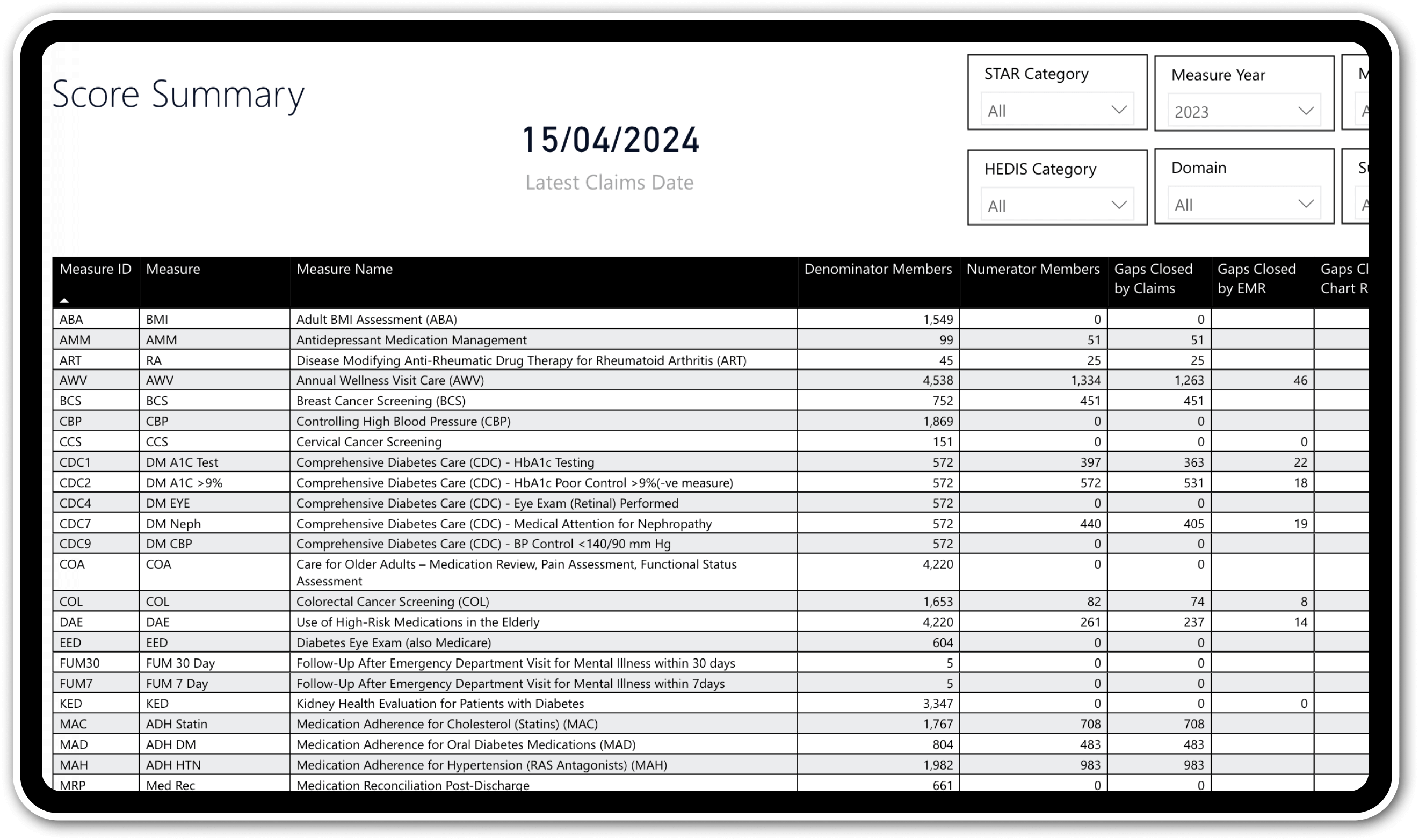
HEDIS & stars tracking & reporting
Track, report, and submit HEDIS and stars measures with confidence, ensuring compliance with regulatory requirements.
360° patient view
Gain a holistic view of patient care by consolidating clinical and claims data in one location, enabling a deeper understanding of quality gaps.
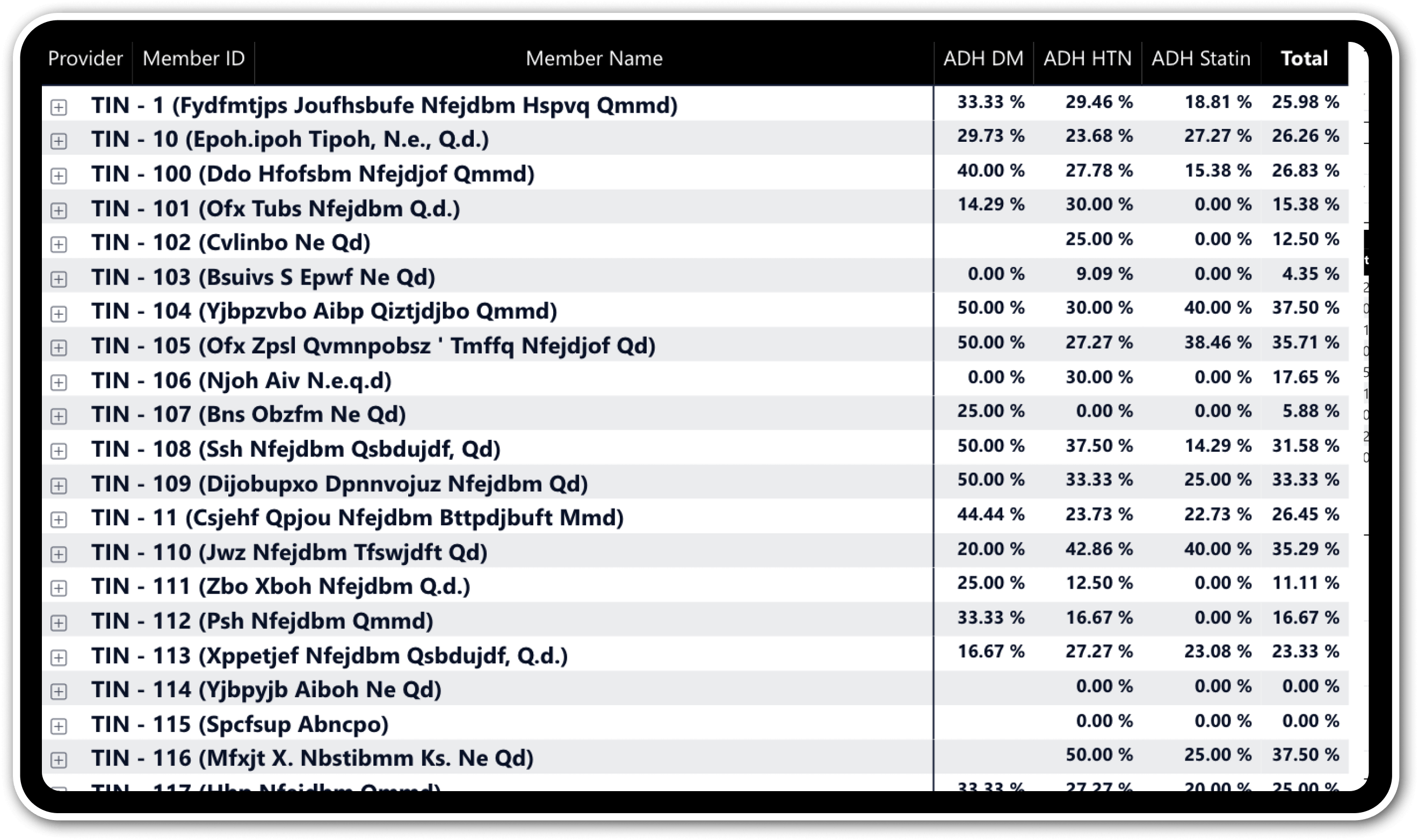
Transparent reporting
Generate comprehensive reports with clear visibility into numerators, denominators, and exclusions, bridging the gap between patients and providers.
State-specific compliance
Ensure accurate and compliant submissions for both national and state-specific quality measures.