IPAs & Physician Groups

Hexplora offers a robust solution for IPAS & PHYSICIAN GROUPS built by leveraging our strong healthcare and technology expertise. Our solution supports the broad ranging requirements of IPAs & Physician Groups covering Data Integration, Business Analytics, Risk Management, and Operational Management. HEXPLORA empowers IPAs & Physician Groups with sophisticated analytical capabilities and enables seamless information exchange with payers and providers. Hexplora platform comes with pre-built interfaces that enable IPAs & Physician Groups to integrate data from different payers into the Hexplora Data Warehouse. From this integrated data warehouse, Hexplora provides a comprehensive overview of their population health, cost, and utilization trends at IPA, Physician Group, Payer, Provider, and individual levels. IPAs & Physician Groups that are transitioning to Risk-based contracts with payers, will succeed or fail based upon their ability to understand and leverage the patient-level data that Payers provide to the IPA & Physician Group for managing risk. Transforming this raw data into meaningful insights is among the most challenging and important tasks that an IPA & Physician Group has. With Hexplora, IPAs & Physician Groups can efficiently track their assigned population each month, identify patient and physician outliers, track quality metrics, drill down on specific disease states, perform ROI analyses, and develop targeted interventions.
HEXPLORA supports the following IPA & PHYSICIAN GROUP requirements:
- Member Tracking
- Provider Engagement
- Quality Management and Reporting
- Plan Reporting
- Risk Management
Member Tracking:
IPAs & Physician Groups can significantly increase their leverage in contract negotiations with payers based on the number of physicians and members that are in their IPA & PHYSICIAN GROUP. This leverage is even more significant in establishing preferred relationships with hospitals, labs, and care and disease management organizations. Hexplora provides comprehensive member tracking functionality both from Enrollment and Clinical perspectives. Enrollment analytics provide pre-built dashboard and reports for monitoring enrollments, dis-enrollments, and member demographics. Clinical analytics include disease conditions by member across time and cost trends.
Provider Engagement:
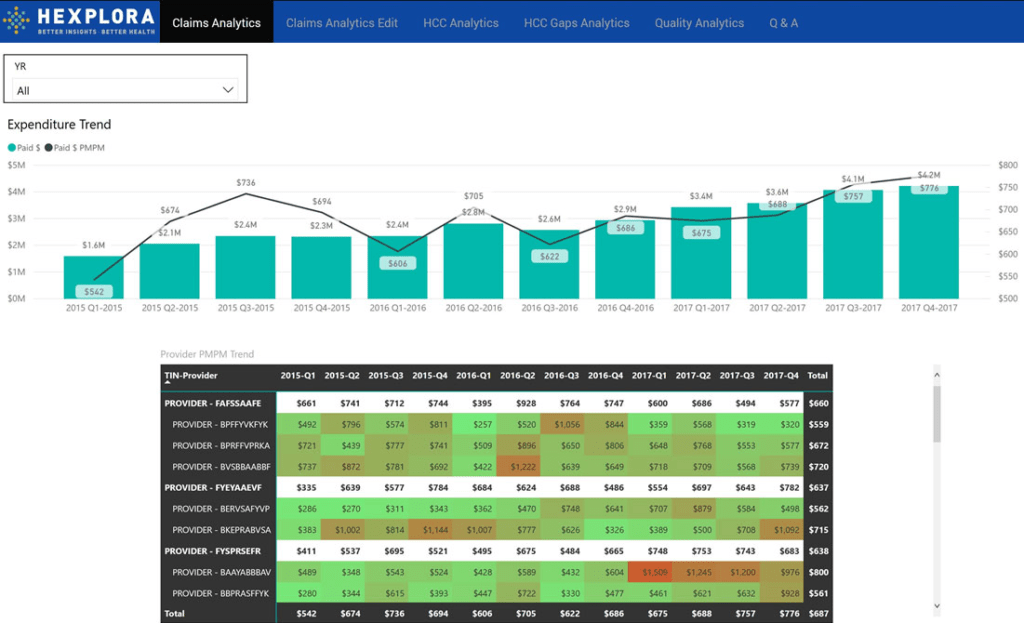
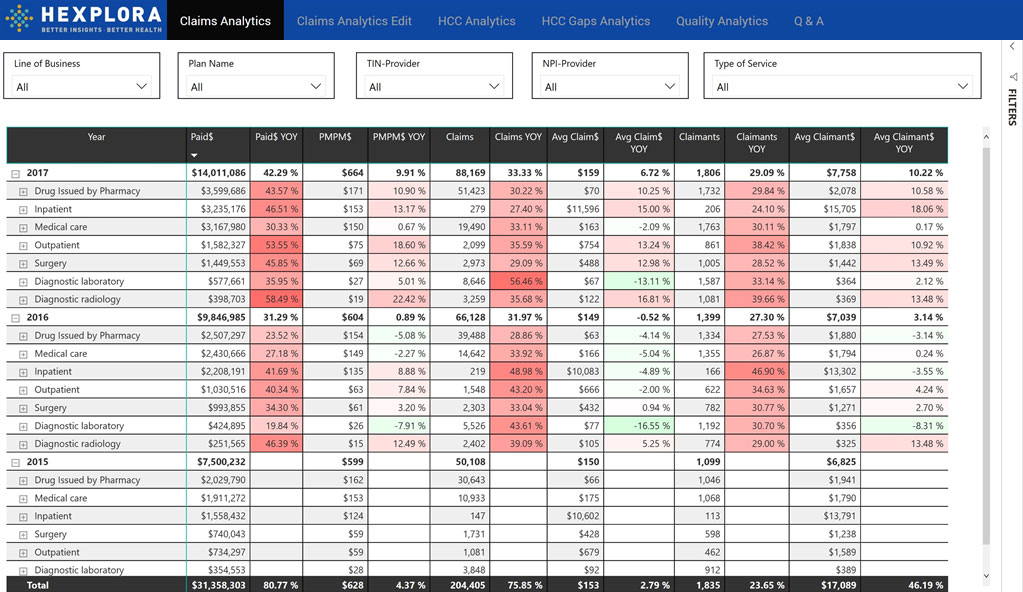
IPAs & Physician Groups are responsible for facilitating coordination and cooperation among providers to improve the quality of care and reduce unnecessary costs. Hexplora empowers the IPAs & Physician Groups through Provider Engagement. PCPs rarely have visibility into the overall healthcare cost for their assigned members. When individual physicians are able to see overall cost and utilization metrics along with a report of their own performance compared to national benchmarks, including, hospitalization rates, re-admission rates, LOS, ER visits, and granular cost data, it is a truly eye-opening experience. All Hexplora Analytics and Reports are available at IPA, sub-IPA, Plan, and individual Physician levels. Individual physicians with access to these reports are able to manage care for their assigned members and reduce the overall cost. IPA management can use the Provider Performance Reports to identify physicians that are not meeting performance measures and individually engage the physicians in implementing provider specific intervention strategies.
Quality Management and Reporting:
Physician Quality and Performance Measurement and Tracking on important dimensions of care and service has become an integral part of the current healthcare environment. Physician Quality Reporting is the basis for incentive payments for EHR Meaningful Use compliance, Medicare and Medicaid reimbursements, and Shared Risk payments at the IPA level. For commercial payers, IPAs & Physician Groups are also required to track and report 75 quality measures across 8 domains of care for HEDIS Performance Measurement.
Data collection of quality measures from individual physicians cannot be a completely automated process for most IPAs & Physician Groups even if all their physicians are on a common EHR platform. Hexplora includes a web based application that provides a guided solution for individual physicians for reporting Quality Measures. Our Quality Management and Reporting solution is an end-to-end solution for collecting data from the individual physicians, validating and aggregating the collected data, and Reporting the aggregated IPA & Physician Group level quality measures to CMS and other Payers.
Plan Reporting:
Most IPA & Physician Group contracts are based on capitated payment models between the payer and providers. In capitated models, providers rarely have a strong incentive to report all the encounters to the payers since there is no encounter level reimbursement. However, payers need to track all the encounters so that they can monitor utilization and quality measures at the plan and provider level. Hexplora provides a comprehensive set of pre-defined reports and interfaces that enable the providers to easily send the data that is requested by the plans on an ongoing basis. Providers are not burdened with creating new processes and reports to satisfy the Plan Reporting requirements allowing them to focus more on providing care to their patients.
Risk Management:
In the changing healthcare landscape, IPAs & Physician Groups are increasingly entering into risk-based contracts with payers, turning the IPAs & Physician Groups into de facto payers, where they directly share risk with the payers in managing their patients’ health and costs. Unlike Medicare ACOs that are based on a standard Shared Savings Model common across all ACOs, IPAs & Physician Groups have to deal with payer specific risk contracts that are further customized for each IPA & Physician Group. Monitoring the IPA & PHYSICIAN GROUP’s performance under each risk contract is a complex task. The problem is compounded when the IPAs & Physician Groups have to deal with multiple contracts across payers. Hexplora provides Risk Management functionality that allows the IPAs & Physician Groups to track each contract and forecast cost and savings trends under each contract and across all contracts.